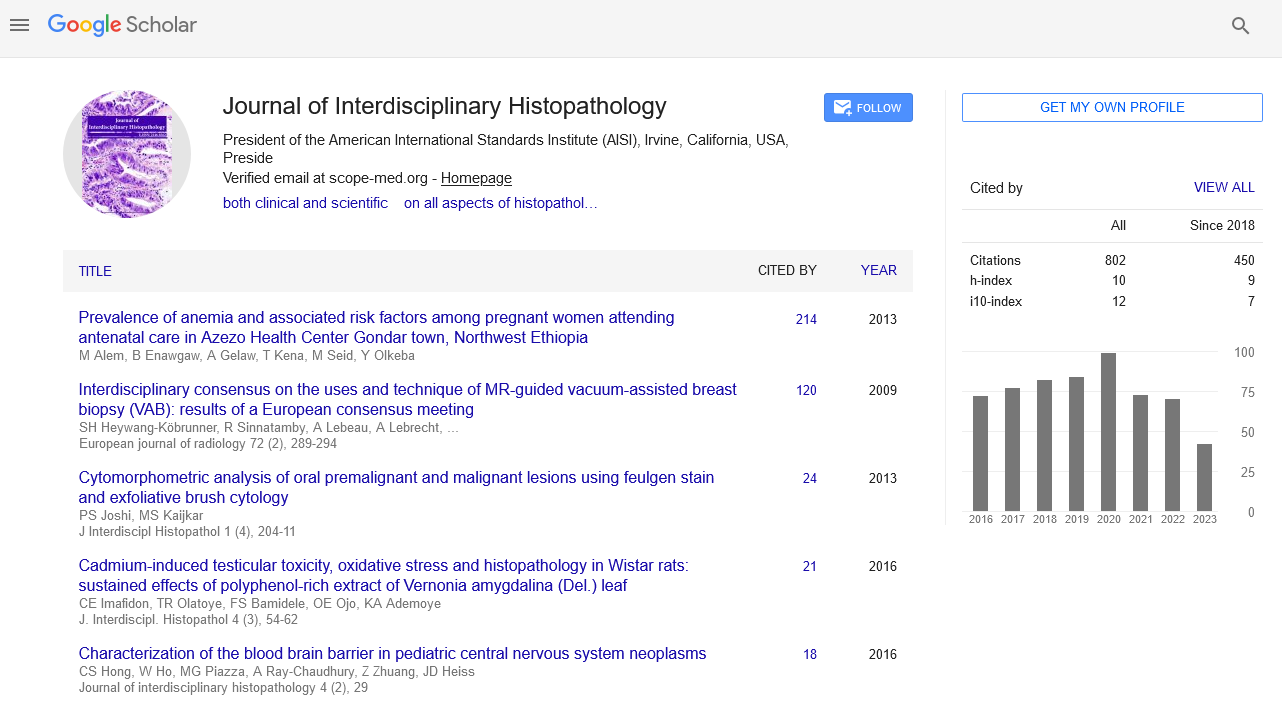
Perspective - Journal of Interdisciplinary Histopathology (2022)
A Note on Mechanism of Cell: Angiopellosis
Roy Arjun*Roy Arjun, Department of Histology, University of Murcia, Murcia, Spain, Email: roy145@gmail.com
Received: 02-Mar-2022, Manuscript No. EJMJIH-22-56181; Editor assigned: 04-Mar-2022, Pre QC No. EJMJIH-22-56181 (PQ); Reviewed: 18-Mar-2022, QC No. EJMJIH-22-56181; Revised: 23-Mar-2022, Manuscript No. EJMJIH-22-56181 (R); Published: 30-Mar-2022
About the Study
Extravasation is a multi-step process that involves cells emigrating from the bloodstream into tissue. Leukocytes, such as T lymphocytes, natural killer cells, neutrophil granulocytes, and monocytes, are the most common extravasating cells. The transfer of cells out of the circulatory system into the surrounding tissue is known as angiopellosis (cell extravasation). Leukocytes (white blood cells) use diapedesis to travel out of circulation; hence this process is unique to non-leukocytic cells. Studying how stem cells reach injured tissue when injected or infused into the bloodstream led to the discovery of angiopellosis. Circulating Tumor Cells (CTCs) have recently been discovered to have the ability to escape blood arteries via angiopellosis during the metastatic process. Angiopellosis is a condition in which the blood vessel wall recognizes cells and then the active remolding of the blood vessel to allow the cell to exit.
When injected intravenously, stem cells have the potential to locate and travel to injured tissue. The cells must pass the blood vessel wall and enter the surrounding tissues in order to exert their therapeutic impact. The extravasation mechanism used by implanted stem cells to escape has yet to be identified. We showed the thorough extravasation processes in vivo for injected stem cells in comparison to white blood cells using intravital microscopy and a transgenic zebrafish strain Tg with GFP-expressing vasculature (WBCs).
When injected intravenously, stem cells have the potential to locate and travel to injured tissue. The cells must pass the blood vessel wall and enter the surrounding tissues in order to exert their therapeutic impact. The extravasation mechanism used by implanted stem cells to escape has yet to be identified.
Mechanism
Extravasation occurs in angiopellosis as a way for cells that are not native to the circulation to leave. Adult stem cells administered intravenously for therapies are included in this category. Normally circulated cells (such as blood cells) either extravasate by diapedesis (white blood cells) or do not extravasate and remain in circulation (red blood cells).
Angiopellosis was discovered by a group of researchers at North Carolina State University who were studying the mechanism intravenously injected stem cells utilized to reach damaged tissue. They discovered that the injected stem cells prompted the blood vessel walls to undergo extensive change on the cellular level which results in the removal of the cell from the inside of the vessel (lumen) into the surrounding area.
Upon entering the circulation, the cell(s) travel through the blood vessels and eventually attach or become lodged inside the blood vessel wall. This prompts the series of events that end in the cell(s) exiting circulation.
The endothelial cells recognize the cell through membrane- specific recognition. Recognition of cell is important and is thought to be the reason cells native to the circulation to not randomly extravasate through angiopellosis.
Once attached or lodged, the exiting cell(s) elicit activity from the endothelial cells of the blood vessel. The endothelial cells extend protrusions and actively remodel themselves around the exiting cells. The exiting cell will then be either actively “pushed” from the inside of the blood vessel, or the vascular cells will remodel around the cell so that the cell no longer remains inside the vessel.
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.