Short Communication - Journal of Interdisciplinary Histopathology (2022)
An Obstacle in Histopathological Diagnosis: Artifacts
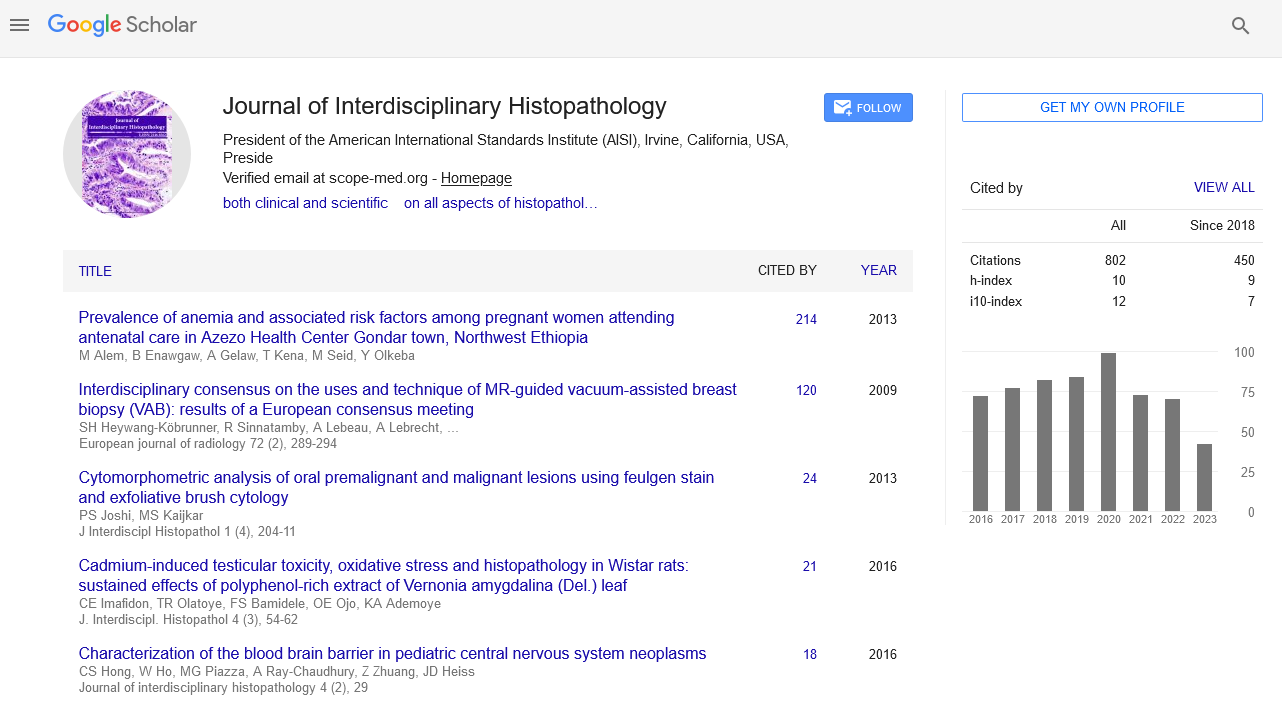
Semin Gedikli* and Ali Can ÖzcanSemin Gedikli, Department of Histology and Embryology, Atatürk University, Erzurum, Turkey, Email: semin.gedikli@atauni.edu.tr
Received: 02-Sep-2022, Manuscript No. EJMJIH-22-73380; Editor assigned: 05-Sep-2022, Pre QC No. EJMJIH-22-73380 (PQ); Reviewed: 19-Sep-2022, QC No. EJMJIH-22-73380; Revised: 06-Dec-2022, Manuscript No. EJMJIH-22-73380 (R); Published: 13-Dec-2022
Abstract
Artifacts are image errors that occur at any stage of tissue from the stage of collection to the stage of staining and create a serious obstacle to reaching a definitive diagnosis in microscopic examination. By distinguishing these artifacts from healthy or pathological tissue, a more accurate definition and subsequently a more appropriate treatment strategy can be determined. With this study, we aim to present some of the artifacts that can be encountered in histopathological examinations used in reaching a definitive diagnosis in the field of health.
Keywords
Artifact; Diagnosis; Histopathology
Description
Histopathology, which is the science of analysis for diagnosis and research, is a science that provides a definitive diagnosis with microscopic examinations and subsequent comments. To reach a definitive diagnosis, the correct selection of the biopsy protocol, fixation, sectioning, and staining stages are important. Negativeness, carelessness, or the presence of a foreign substance in any of these stages can lead to error in the analysis. These errors, which are sometimes encountered in these examinations, where even the smallest detail is important, are called “artifacts” [1]. The term artifact used for histopathological examinations is the name given to the change of structure or tissue as a result of a foreign factor in a microscopic section [2]. Various factors such as problems in fixation fluids, insufficiently fixed tissues, and tissues kept in excessive heat or cold, mistakes in surgical intervention, exposure to chemicals, locally applied anesthetics, and not applying the correct staining protocol cause artifacts [1]. While some artifacts can be easily distinguished, some artifacts are difficult to distinguish, which may lead to errors in diagnosis [3]. Artifacts are classified as Prefixation artifacts, fixation artifacts, and tissue-processing artifacts, artifacts related to bone tissue, artifacts related to microtomy, staining artifacts, artifacts related to floatation and mounting artifacts [2]. This article focuses on artifacts encountered during Prefixation and fixation.
Types of artifacts
Prefixation artifacts: The type of artifact that occurs before the fixation stage is called Prefixation artifact. These types of artifacts can occur after blade damage, crushing during a surgical procedure or contamination during surgery. Such artifacts can be prevented by raising the awareness of those responsible for this procedure [4].
Injection artifacts: It is an artifact that occurs as a result of intraregional aesthetic solution injections, which can cause bleeding and vacuolization as a result of the separation of connective tissue bands. Direct administration of aesthetic to the lesion should be avoided, local anesthetics should be applied only if the area is large enough for the lesion [1,4]. It has also been reported that aesthetic solutions administered in large amounts may cause bleeding that disrupts the integrity of the cellular structure [4].
Squeeze artifacts: It is a type of artifact that occurs due to the pressure of the tissue by surgical instruments such as crushing, bleeding, and fragmentation. Tissues are damaged even if they are slightly compressed. If the surgical instrument used has serrations, these serrations cause tears in the sample. Exposing the samples to such pressure and subsequent destruction causes the loss of cytological details [1,2]. In addition, various electrodes such as electrocautery used to prevent bleeding during a biopsy can cause such artifacts [4].
Fulguration artifacts: It is a type of artifact encountered as a result of the change of connective tissue and epithelial tissue as a result of high temperature. It occurs as a result of heat emitting instruments such as electrocautery and laser, creating a thermal necrosis area. It results in the separation of epithelial and connective tissue from each other and the nuclei becoming spindled. On microscopic examination, the tissues appear to have a clotted and torn appearance [1,2]. It is an artifact characterized by a more opaque and amorphous appearance of fibrous connective tissue, muscle, and fat. This situation can be avoided by using heat dissipating surgical instruments at lower milliamperes and choosing instruments produced by combining surgical blades with electricity [4].
Tattoo pigment artifacts: Tattoo, which is becoming more and more widespread in our age, leaves an insoluble colored residue on the skin pigments due to some chemicals in them. Although no reaction is usually encountered, it is reported as an artifact type as it may lead to a fallacy in diagnosis [4].
Autolysis artifact: For the diagnosis to be made correctly, correct fixation should be performed without losing tissue vitality. Vacuoles are likely to be encountered in the cytoplasm of autolyzed tissue, and nuclear changes that may be encountered include pyknosis, karyolysis, and karyorrhexis [2].
Improper prefixation: Fixation of the tissue is provided by passing through various series of solutions. Solutions such as normal saline do not fix the tissue, on the contrary, since the tissue will autolyze over time, it may cause great errors in the diagnosis [2].
Fixation artifacts
To obtain a healthy microscopic image from the tissues, proper tissue diffusion must be ensured and tissue layers must be prevented from separating from each other. Fixation can be considered the first step of the histological and cytological examination. Fixation is a step that helps the tissue taken from the living thing to be examined as close to its original state [5]. Generally, 10% diluted formaldehyde is used for the fixation of tissues and formaldehyde shrinks tissues by 33%. In addition, it has been reported that nuclei appear larger in microscopic examination of frozen tissues [1,4]. While the concentration of the fixative agent used and the fixation time cause various errors in sectioning, various blots may be encountered in microscopic examinations due to the content of different fixative agents [4].
Shrinkage artifacts: Shrinkage artifacts, which are one of the most common artifacts, are formed as a result of shrinkage or growth of tissues. While the tissues are taken and fixed, some differences in membrane permeability occur. Due to these differences, some layers in the tissues can separate from each other and this can lead the researcher to a mistake in diagnosis [4].
Microwave fixation artifacts: In some histopathological staining protocols, microwave fixation is provided. Microwave, which has been accepted in histopathological protocols in recent years, has been used in various stages such as stabilizing tissues, frozen techniques, fixation, staining, histoprocessing, and immunotechniques [6]. High temperatures should be avoided while providing fixation with the microwave. The optimum temperature for fixation is in the range of 45-55 degrees, and as a result of exceeding 65 degrees, vacuolization, an over-stained cytoplasmic appearance, and pycnotic nuclei can be encountered. On the contrary, if fixation is attempted with insufficient heating, the microscopic image quality will be seriously affected [2,4].
Streaming artifacts: This type of artifact, which is frequently seen in tissues fixed with formaldehyde, is a type of artifact that occurs when it is localized in a different place from its original place, due to the diffusion of materials that have not been fully fixed. It is possible to prevent this situation by using glycogen fixatives or freeze-drying processes [2,4].
Diffusion artifacts: It is a type of artifact defined by the loss of small molecules such as inorganic ions, cofactors, and biogenic amines, which are formed as a result of some materials in the tissues not being trapped inside and spreading out of the tissue. This artifact should be considered, especially in cases where enzyme histochemistry is examined [1,4].
Ice-crystal artifacts and freeze artifacts: If fixation is to be achieved with a freezing protocol, fixation of the tissue should be ensured by making an isopentane bath cooled to -160to-180 degrees with liquid nitrogen, and it should be known that ice crystals will form unless the tissue is completely frozen. The formation of ice crystals causes the tissue to become unrecognizable and thus prevents the diagnosis from being made correctly. As a result of taking large tissue samples, this artifact occurs because the tissue does not freeze at the desired level in the specified time. In addition, freezing of the solution during fixation as a result of choosing the wrong fixative solution will also cause this artifact [2,4].
Osmolality of the fixative solution: The osmolality of the preferred fixation material causes swelling of cells or increased extracellular spaces. Fixation materials, which are preferred as isotonic and hypotonic, cause deplasmolysis of cells and thus lead to misdiagnosis. It is possible to prevent such artifacts by using hypertonic fixation products [2].
Conclusion
As a result, although histopathological diagnoses made for various purposes such as procedures to shed light on scientific studies in experimental animals and to confirm the diagnosis in biopsy allow us to apply more appropriate treatment protocols for service to humanity, the correct diagnosis and correct treatment principle may not be applied as a result of some artifacts encountered. It is important to identify artifacts and ensure that they are minimized with the measures taken, and in addition to these, it is important to determine what kind of diagnostic protocol to follow in the presence of artifacts.
References
- Chatterjee S. Artefacts in histopathology. J Oral Maxillofac Pathol 2014; 18: S111-S116.
[Crossref] [Google Scholar] [Pubmed].
- Taqi SA, Sami SA, Sami LB, Zaki SA. A review of artifacts in histopathology. J Oral Maxillofac Pathol 2018; 22: 279.
[Crossref] [Google Scholar] [Pubmed].
- McInnes EF. Artifacts in histopathology. Background Lesions in Laboratory Animals: A Color Atlas. New York: Saunders Elsevier 2011.
- Ekundina VO, Eze G. Common artifacts and remedies in histopathology (a review). African Journal of Cellular Pathology 2015; 4: 1-7.
[Crossref] [Google Scholar].
- Dey P. Fixation of histology samples: Principles, methods and types of fixatives. Basic and advanced laboratory techniques in histopathology and cytology 2018; P: 3-17.
[Crossref] [Google Scholar].
- Mathai AM, Baliga P, Rai S, Naik R. Microwave histoprocessing versus conventional histoprocessing. Indian J Pathol Microbiol 2008; 51: 12-16.
[Crossref] [Google Scholar] [Pubmed].
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.