Mini Review - Journal of Interdisciplinary Histopathology (2022)
Human Amnion/Chorion Membrane Use During Neck Surgery to Protect the Recurrent Laryngeal Nerve
Gary Clayman*, Rashmi Roy and Nathaniel WalshGary Clayman, The Hospital for Endocrine Surgery, The Thyroid Institute, Tampa, FL, USA, Email: clayman@thyroidcancer.com
Received: 21-Apr-2022, Manuscript No. EJMJIH-22-61382; Editor assigned: 22-Apr-2022, Pre QC No. EJMJIH-22-61382 (PQ); Reviewed: 06-May-2022, QC No. EJMJIH-22-61382; Revised: 13-May-2022, Manuscript No. EJMJIH-22-61382 (R); Published: 23-May-2022
Abstract
Recurrent Laryngeal Nerve (RLN) damage is a significant and prevalent complication of neck surgery of all types. Based on the beneficial role of Human Amnion/Chorion Membrane (HACM) allograft in wound management and nerve regeneration, we investigated whether placement of a commercially available HACM allograft on dissected RLN during thyroidectomy could reduce the occurrence and/or duration of RLN. Preliminary studies in 100 dissected nerves showed benefit in both occurrence and duration, so the study was increased to 1000 consecutive at-risk nerves (dissected exposure of at least 3 cm of RLN) in 670 patients which received HACM directly onto the nerves prior to wound closure. 2000 at-risk nerves without HACM in 1420 matched patients served as controls. All operations were performed by the same surgeons using nerve monitoring endotracheal tubes. Patient-reported vocal analysis, physician-assessed vocal analysis, and laryngoscopic assessment of vocal fold dysfunction were performed before and after surgery. The overall incidence of clinically significant RLN injury at 24 hours after surgery in patients not receiving HACM was 14.4% which decreased to 3.4% in the HACM-treated group (p<0.01). Moreover, the time to resolution of documented RLN decreased from 8.9 weeks to 4.0 weeks (p<0.01). Intraoperative placement of HACM allograft over at-risk RLNs during thyroidectomy appears to decrease both the incidence of and duration of RLN injury, which could address the most significant complication in head and neck surgery.
Keywords
Recurrent laryngeal nerve; paralysis; thyroid; amniotic allograf
Introduction
The Recurrent Laryngeal Nerves (RLNs) innervate intrinsic muscles of the larynx that act to open, close, and adjust tension of the vocal cords. The RLNs also carry sensory information from the mucous membranes of the larynx below the lower surface of the vocal fold, as well as sensory, secretory, and motor fibres of the trachea and esophagus. These nerves often are injured during surgical procedures on the thyroid and parathyroid glands but also are at risk during other neck surgical procedures. To reduce the risk of injury to these nerves during surgery, it is conventional to first identify and dissect them so that they can be protected during subsequent surgical activities. Despite experience, diligence, and the most careful attention of the surgeon, transient or permanent injury to the RLNs occurs in 0.5% to 30% of all thyroid and parathyroid operations. More extended resections, including bilateral neck dissections, carry an even greater risk of nerve injury.
Inadvertent iatrogenic damage to the RLNs induces a temporary or permanent paresis or palsy of the ipsilateral vocal cord and can lead to dyspnea and problems with deglutition. Simply touching or rubbing the nerve during dissection can result in paralysis of several months and occasionally permanently. Patients who experience an intraoperative RLN injury typically experience dysphonia for a minimum of 10 to 12 weeks, with approximately 8% to 10% having a permanent injury that does not improve with even extended time. Being unable to protect the trachea, these patients frequently aspirate liquids.
Attempts to decrease the risk of intraoperative nerve injury have been limited to conversion to less extensive surgery or use of nerve monitoring endotracheal tubes despite the lack of peer-reviewed effectiveness data. A commercially available Human Amnion/ Chorion Membrane (HACM) allograft has been shown to serve as a protective barrier during wound healing. It is also known to provide multiple extracellular matrix proteins, growth factors, cytokines, and other specialty proteins that inhibit scar formation and dramatically improve injured nerve function in animal studies, and to promote healing of skin, tendons, nerves, and corneal wounds and significantly impact soft tissue repair in human clinical trials. In the clinical study described herein, we began to investigate the hypothesis that intraoperative placement of an HACM allograft directly onto dissected nerves might reduce the incidence, severity, and/or duration of intraoperative RLN injury. This first study was not designed to investigate the mechanism(s) through which any protective effect might be mediated, such as a protective barrier function provided by the allograft and/ or any biologic activities inherent in the allograft material, but these questions would become a significant priority if HACM placement suggested a protective effect on nerves dissected during surgery.
For as long as surgeons have been operating in the neck, the most feared complication for both patient and doctor has been transient or permanent injury to the recurrent laryngeal nerve. A paralyzed vocal cord nerve is often devastating to the patient who cannot phonate well inhibiting their ability to communicate and work, but most also have problems protecting their airway and often aspirate liquids and thus have difficulties eating [1]. Although the rate of nerve injury is directly related to the extent of the dissection and the experience of the surgeon, it is estimated to occur in over 175,000 patients per year in the US with a huge societal cost. Despite countless technical innovations in the operating room over the past 50 years, the rate of nerve injury has not decreased [2,3].
The development of nerve-monitoring endotracheal tubes was envisioned to address the rate of nerve injury, but the vast majority of published studies show no decrease and occasionally, an increase nerve injury rate when the surgeon puts too much emphasis on the tube and not enough in the finer aspects of the dissection [4]. Despite nerve monitoring being considered standard of care for many neck and thyroid operations, surgeons generally don’t believe the technology helps and they have resorted to using it primarily to help avoid the most frequent malpractice claim should a nerve be injured and not every step was taken to help avoid the injury.
As the world’s highest volume thyroid/parathyroid surgery center, we have a tremendous amount of experience dissecting the neck and have unparalleled experience with the recurrent laryngeal nerve. Yet we are not immune to nerve injuries, which are typically transient in our hands, yet still lasting about 3 months on average. In nearly 100% of cases, the nerve is completely intact at the completion of the operation-yet it can develop a neuropraxia preventing successful propagation of the nerve impulse. The cost of this injury, even when transient, cannot be overstated. It is a major problem for the patient as well as the managing physician and his/her office staff.
A new way of thinking: Biologics
We began looking at neuropraxia as a wound injury and wondered if we could apply some of the new biologic membranes that have revolutionized chronic wound care. Human Amnion/Chorion Membrane (HACM) has become standard of care for many non-healing diabetic ulcers and other wounds that have had the normal wound healing cascade inhibited for a number of reasons. We hypothesized that our physically intact and uninjured to even the magnified eye, had its normal healing process inhibited as well. We hoped that applying HACM directly to a dissected nerve would hasten its recovery from being manipulated, and possibly decreasing a 3-month healing process to a significantly shorter time.
Human amniotic membrane has been known for a number of years to contain biologically active proteins that may be beneficial to patients with various chronic wound problems. The literature is full of studies showing over 100 different growth factors, cytokines, anti-inflammatory mediators and other proteins to be present within the HACM which are then exuded into the tissues to which it is applied [5,6].
HACM is donated by mothers and harvested from C-section live births, processed to contain the amniotic membrane only, or both the amnion and Chorion layers. It is then dehydrated, sterilized, and cut into sheets that typically measure from 3 cm x 3 cm to 10 cm x 15 cm. Amnion by itself is very thin (typically only one or two cell layers thick) and once rehydrated is difficult to work with. The combination of amnion/Chorion is thicker, like wax paper, but still translucent, becoming transparent when it is rehydrated after being placed on a wound. The tissue is immune privileged, meaning it has no antigenic properties and thus any untoward reaction to the material is essentially unknown and unreported.
Our clinical trial and unexpected results
Our recent publication in Cell Transplant [7] outlines our initial use of HACM in 67 patients undergoing thyroid cancer surgery with neck dissection who had 100 fully dissected (>3 cm of nerve length) recurrent laryngeal nerves treated by laying HACM directly over the entire exposed nerve surface like a blanket. The HACM was left in situ covering the nerve when the wound was closed. The control group was 205 similarly dissected nerves in 134 patients who were matched for age, gender, type of cancer, number of neck lymph nodes removed, and duration of surgery. Importantly, the same two very high-volume thyroid surgeons (GC, RR) performed every operation.
Patients were monitored for all possible manifestations of RLN injury, including dysphonia, aphonia, difficulty breathing, and difficulty swallowing. All patients had endoscopic visualization of vocal cords prior to, and 24 hours after surgery, and at later time points as long as symptoms of nerve injury remained. All post-operative findings in both groups were limited to vocal changes which were scored based on the subjective patient-reported vocal analysis scale, physician assessment of vocal changes, and laryngoscopic assessment of objective vocal fold dysfunction.
HACM application decreased both the incidence and duration of nerve injury following thyroid cancer surgery. We hypothesized that the duration of nerve injury would be shortened due to the contained growth factors (e.g., HGF, ILGF, EGF) and anti-inflammatory agents present (e.g., IL1-Ra) and this was shown in the data whereby the median time to recover was decreased from 4.5 weeks to 10 days. What was surprised us, was that the overall incidence of transient nerve injury decreased from 12.5% to 1.8%. This was not expected, and because the injuries are defined/ detected on the first day after surgery, we hypothesized that a secondary mechanism of action was in play as this is likely to be too quick for any pro-growth and pro-healing mediators to be at work. HACM is known to exude IL1-Ra, a potent anti-inflammatory and anti-scarring compound (among others) and thus rather than promoting healing, it may be that the immediate prevention of inflammation and recruitment of inflammatory cells (macrophages, etc) that is playing a role in the decrease in overall incidence of the injuries.
As we correlated our findings with other studies in the literature, we realized that the physical barrier function of the HACM may be playing a major role in the prevention of nerve injuries-rather than hastening their repair. By the nature of the dissection, the recurrent nerve is exposed and laying on the surface of the deep aspect of the wound. When the wound is closed, the muscles of the neck, primarily the sternocleidomastoid and strap musculature are put into direct contact with the exposed nerve, such that every movement of the patient’s head results in a rubbing and irritation of the nerve surface. The physical barrier function of HACM has been widely described in other applications (e.g., burns) and we believe plays a major role in this application as well.
Change in our standard of care
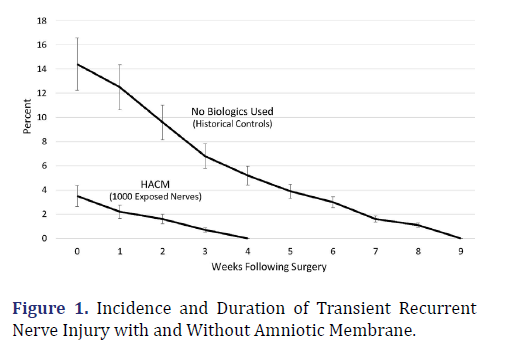
Because of the results of this study, the use of amniotic membrane became standard practice for all exposed recurrent nerves at the Hospital for Endocrine Surgery. This includes the near 4000 parathyroid operations performed annually as well, although parathyroid surgery does not require dissection of the recurrent laryngeal nerve very often, compared to nearly all cases of thyroidectomy. Now that we have used HACM in over 1000 cases where the nerve is completely dissected for >3 cm, our incidence of nerve injury remains at an all-time low around 3% compared to 13%-16% over the past 30 years of our practice here, and previously at MD Anderson Cancer Center, Yale, Cleveland Clinic, Harvard, USF, Princeton, and the other institutions where our surgeons have practiced and performed these operations.
Figure 1 illustrates the difference in both incidence and duration of nerve injury where we compare historical data from thousands of our patients where intraoperative nerve monitoring was used exclusively, to the same operation performed by the same surgeons using HACAM on every dissected nerve (n=1000). Aside from a lower rate of injury which would be a significant advancement by itself recovery of nerves that do show signs of neuropraxia postoperatively continues to be more than twice as fast as historical controls.
Similar results were published by Dr Tobias Carling at Yale University Medical Center in 2021 where application of HACM to fully dissected recurrent laryngeal nerves during thyroidectomy provided a quicker return of nerve function in injured nerves [8]. He also showed a decreased incidence of injury but was unable to show statistical significance because of the small number of affected individuals.
The surgeons at the Hospital for Endocrine Surgery in Tampa, Florida have made application of HACM standard of care for all exposed recurrent laryngeal nerves regardless of the underlying disease or type of operation performed. We believe this to be the most significant advancement in this field in more than 50 years and expect this technique to be adopted throughout the surgical management of all “at risk” patients in the near future regardless of the type of neck surgery being performed.
Conclusion
Application of human amniotic membrane to 1000 consecutive, fully dissected (>3 cm) recurrent laryngeal nerves during thyroidectomy provided significant benefit in both incidence and duration of transient nerve injury compared to historical controls which had nerve monitoring performed, but without application of amniotic membrane as a protective covering and source of biologic proteins.
Conflict Statement
Drs Clayman, Roy, and Walsh have no financial interest, consulting agreement, or undisclosed conflict to report. An affiliated surgeon at the Hospital for Endocrine Surgery has applied for patent protection of HACM use on RLN.
REFERENCES
- Misono S, Peterson CB, Meredith L, Banks K, Bandyopadhyay D, Yueh B, et al. Psychosocial distress in patients presenting with voice concerns. J Voice 2014;28:753-761.
[Crossref] [Google scholar] [PubMed]
- Bergenfelz A, Jansson S, Kristoffersson A, Martensson H, Reihner E, Wallin G, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg 2008;393: 667–673.
[Crossref] [Google scholar] [PubMed]
- Bergenfelz A, Jansson S, Kristoffersson A, Martensson H, Reihner E, Wallin G, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg 2008;393: 667–673.
[Crossref] [Google scholar] [PubMed]
- Koob TJ, Rennert R, Zabek N, Massee M, Lim JJ, Temenoff JS, et al. Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J 2013;10:493-500.
[Crossref] [Google scholar] [PubMed]
- Kogan S, Sood A, Granick MS. Amniotic Membrane Adjuncts and Clinical Applications in Wound Healing: A Review of the Literature. Wounds 2018;30: 168-173.
[Crossref] [Google scholar] [PubMed]
- Kogan S, Sood A, Granick MS. Amniotic Membrane Adjuncts and Clinical Applications in Wound Healing: A Review of the Literature. Wounds 2018;30: 168-173.
[Crossref] [Google scholar] [PubMed]
- Carling T. Protection of laryngeal nerve palsy using amniotic membrane shield during thyroid surgery. Endocrine 2021;74:197-199.
[Crossref] [Google scholar] [PubMed]
- Alesina PF, Rolfs T, Hommeltenberg S, Hinrichs J, Meier B, Mohmand W, et al. Intraoperative neuromonitoring does not reduce the incidence of recurrent laryngeal nerve palsy in thyroid reoperations: results of a retrospective comparative analysis. World J Surg 2012; 36:1348-1353.
[Crossref] [Google scholar] [PubMed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.